ERA & Payments Posting
This document details how the Electronic Remittance Advice (ERA) is downloaded to CharmHealth from the Clearinghouse in different ways, how it can be viewed in CharmHealth, and how the payments are posted to the Claims.
- Electronic Remittance Advice
- Downloading ERA
- Manual ERA File Upload (ANSI 835 File)
- ERA Download History
- ERA Views
- ERA Payment Posting Settings
- Ability to Review the Applied ERA Payments
- Ability to Review the ERA and Initiate Payment Posting
- Option to Download 'ERA 835' File
- Enhancements in ERA Payment Posting
- Enable Item Level Payments to Invoices
- Configure Role-Based Access to ERA
- Delete an ERA
Electronic Remittance Advice
Electronic Remittance Advice (ERA) is an electronic form of claim payment information from the Payer with the Explanation of Benefits (EOB) details.
Downloading ERA
ERAs get automatically downloaded to CharmHealth as and when it is available in the Clearinghouse system. Optum users have an option to download the ERAs for a given period.
For Optum Clearinghouse users,
Automatic Download
By default, the ERA download process is automated. You can change the frequency and time of download under the 'Settings > Billing-eClaims > ERA Settings' section.

Manual Download
- If there is a need to download ERA manually, click on the 'Download ERA' button under the 'Billing > ERAs' section.

- Clicking on the 'Download ERA' button opens the 'ERA Download' dialog box.
Choosing the date and clicking the 'Download ERA' button connects to the Optum server and downloads the available ERAs in the selected period. Once the ERAs get downloaded, a summary of downloaded ERAs is shown.

For ChangeHealthcare Clearinghouse users,
The ERAs get automatically downloaded to the CharmHealth system, and no special configuration is required.
Manual ERA File Upload (ANSI 835)
When a payer is not supported by the Clearinghouse and can obtain ANSI 835 files from the Payer portal, Charm offers an option to upload the 835 files using the 'Upload ERA (ANSI 835)' option.

When an ERA is uploaded, CharmHealth will process and match the EOBs with the invoices and post the payments.

ERA Download History
The ERA download transactions are listed under the 'Billing > ERAs > ERA Download History' section.

ERA Views
The downloaded ERAs can be viewed in the 'Billing > ERAs' section.
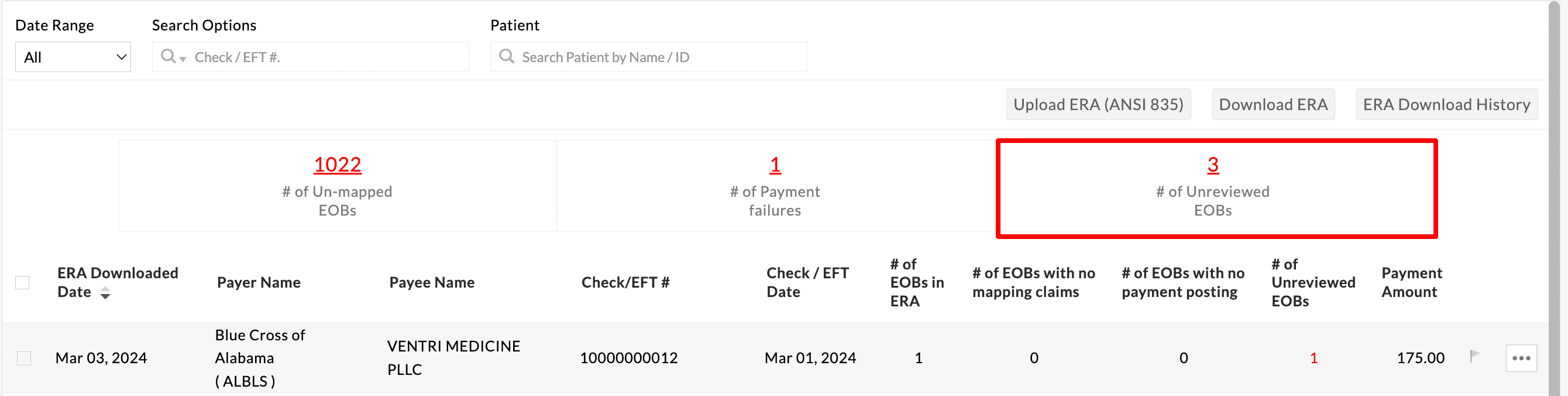
ERA List View and Summary
A list of ERAs appears with details such as ERA Downloaded Date, Payer name, Payee name, Check/EFT number, and Check/EFT date.

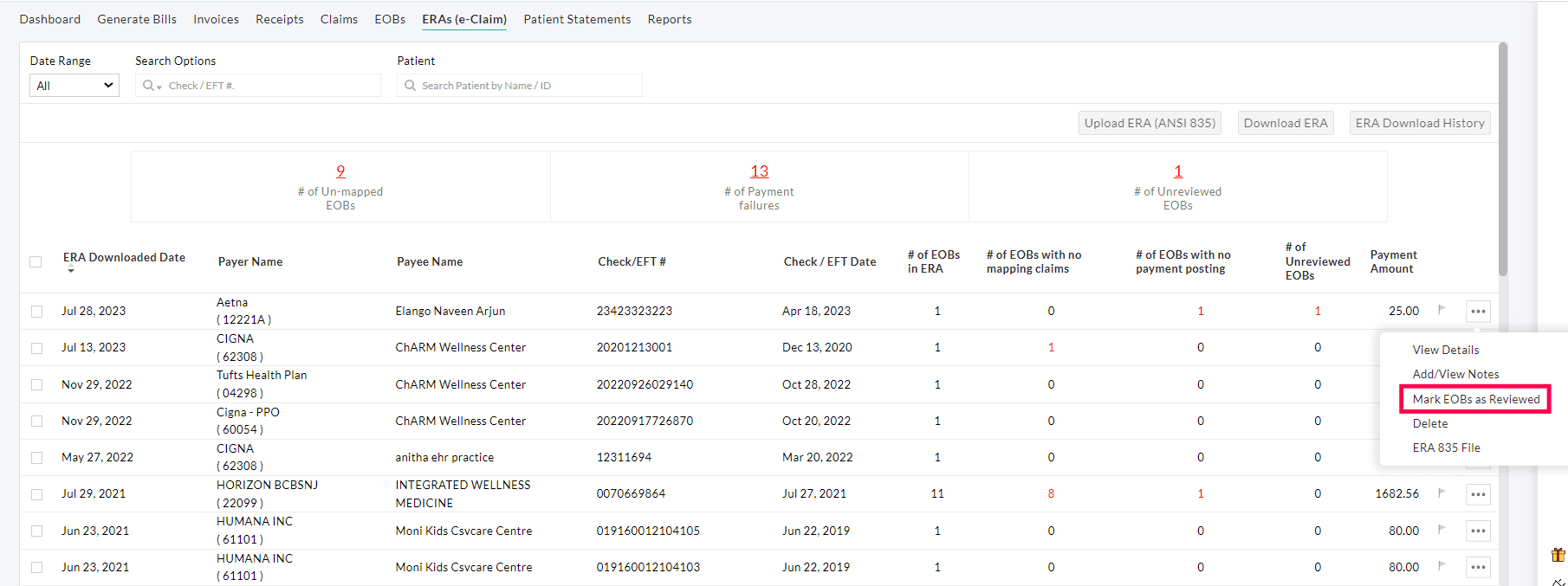
A summary of all ERAs downloaded is shown in the ERA Watchlist with the number of Unmapped EOBs, Payment failures, and Un-reviewed EOBs.
| Unmapped EOBs | EOBs for which CharmHealth could not find matching Claims. It means that either the Claim is not created in CharmHealth but submitted from some other system, or the Claims are available in CharmHealth, but our standard algorithm has failed to find it. You can use the filter option to filter the unmapped EOBs. |
| Payment failures | EOBs for which applying Claim payments failed. Practice can apply for these payments manually. You can use the filter option to filter these failures. |
| Un-reviewed EOBs | EOBs for which the manual review is required for successfully applied payments. Practice can list the EOBs to verify the ERA payments applied and mark them as reviewed. |
Detailed ERA View

Click on an ERA from the list to see the detailed view. This view shows the following information:
- Payer and Payee details
- Payment details - Check number, Check date, Method of payment, and Amount
- ERA Provider Adjustment - It is the amount such as credit interest, late payment penalty, etc., as per the contract between the Payer and Provider. It may not be related to a specific Claim or service.
- EOB Summary - List of EOBs present in the ERA.
- EOB Details - The EOB view contains payment/adjustment information as given by the Payer.
Fixing EOB Mapping Failure
CharmHealth finds a matching Claim for an EOB with the following details of the EOB, such as Patient Control Number, Date of Service, and first CPT in EOB. When the EOB gets mapped to a claim, the respective Invoice ID is shown above the EOB.
Sometimes, CharmHealth may fail to identify the Claim of an EOB. This means, either the Claim for that EOB is created and submitted from some other system, or the logic used for Claim mapping fails to identify the Claim. In such a case, an error message gets displayed above the EOB. Refer to the below screenshot.

If the actual Claim is created in CharmHealth, then the user can find the Claim and map it to the EOB using the 'Select the Claim for this EOB' option. Clicking this option shows a list of Claims matching with the Patient's name shown in the EOB. Users can verify the list, select a particular Claim, and map it by clicking the 'Match Claims' button.
If there is no Claim in CharmHealth for the EOB received, it can be marked as EOB with no matching Claim using the 'Do not show this message. This EOB does not have a matching Claim' option.
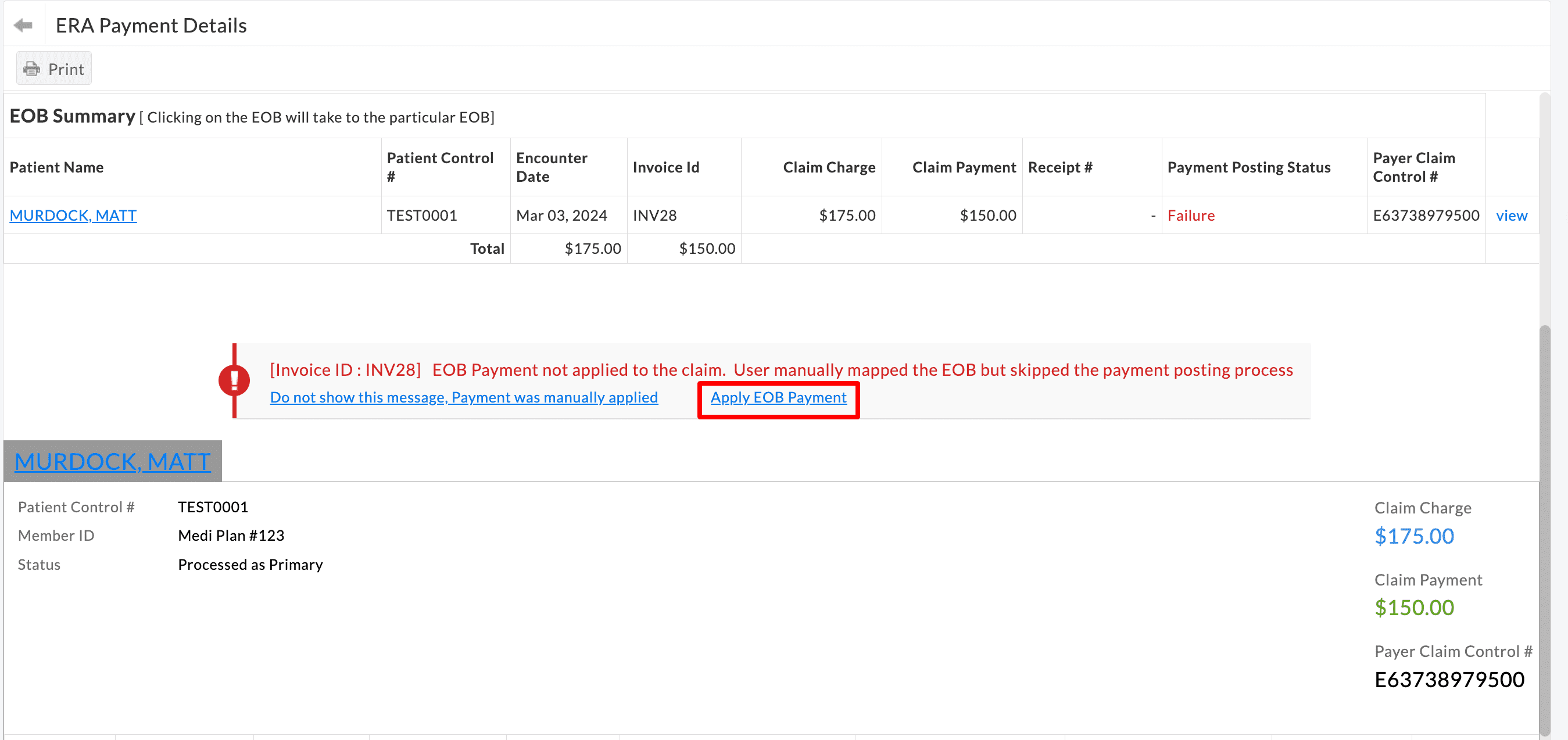
Fixing Payment Posting Failure
If a Claim is mapped to an EOB, and there is an error in applying the payment automatically, a message gets displayed with the reason for failure. In such a case, the user has to apply the payments manually. Once the payments are applied, this error can be cleared by clicking the 'Do not show this message again, Payment was manually applied' option.

View EOBs Mapped to Claim
To view all the claims that have EOBs, use the 'Has EOB' filter. This will filter all claims that have received EOBs from the payer.

To view EOBs of a claim click on the 'More Options(...) > Show EOB (2)' option. Here, 2 indicates the number of EOBs received for the claim. The EOB Details view has the option to print the EOB and Export it as PDF.


ERA Payment Posting Settings
Automatic Claim mapping and payment posting can be controlled under the 'Settings > Billing-eClaims > ERA Settings' section. The options available under ERA settings are explained below.

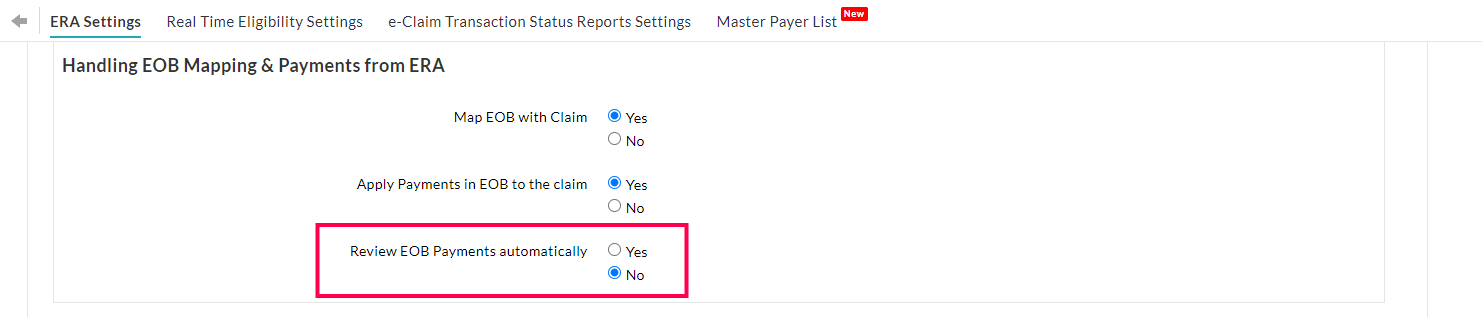
Handling EOB Mapping & Payments from ERA
| Map EOB with Claim | This option automatically maps the EOBs received through ERA payments to their respective Claims.
If 'Yes' is selected, which is a default setting, the EOBs get mapped to their Claims automatically.
If 'No' is selected, EOBs get downloaded and listed, but they will not be linked to any specific Claim. Practices should manually map the EOBs with the Claims. |
| Apply Payments in EOB to the Claim | This option applies the EOB payments to the corresponding Claims.
If 'Yes' is selected, which is a default setting, the payments get applied to the Claims automatically.
If 'No' is selected, Claim payments will not be applied. This option should be chosen when the Practice needs to add payments manually or wants to review the details in the ERA before applying the payment.
To automatically apply for Claim payments, ensure that the 'Map EOB with claim' setting is enabled. |
| Review EOB Payments Automatically | This option allows Practices to review the EOB Payments that are automatically applied from ERA.
Selecting 'Yes' will automatically mark the EOB Payments as reviewed when applied from ERA.
On choosing 'No', the review can be done manually for the payments added from ERA.
To learn how to review ERA payments manually, Click Here. |
Payment Reversals
| If EOB has Reversal payments, then | The 'Apply Values as given in EOB' option applies the reversal payments to the Claim as given in the EOB.
The 'Do Nothing' option is selected by default, which will not apply any payment when there is an EOB with a negative payment. |
Handling Denials
| If any CPT line in EOB has Zero Payment without Copay, Co-insurance, and Deductible, then | The 'Mark CPT as Denied' option is selected by default, which marks the CPT line as denied if it has zero payment without Patient Responsibility types like Copay, Co-insurance, and Deductible.
If the 'Apply values as given in EOB' option is selected, a payment amount of zero gets added to the CPT. |
Secondary Claim Payments
| If ERA has payments from the Secondary payer, then | When the primary Claim is submitted to the secondary payer as a crossover claim along with the EOBs (i.e., COB) by the primary payer itself, the secondary payer will process the claim and send the secondary EOB. In that case, choosing the option 'Apply Payment Always' will apply the payment from the secondary EOB to the available claim if the secondary claim is available, or else to the primary claim. Choosing the other option 'Apply Payment only when Secondary Claim is available' will post the payment only to the secondary claim, if available. |
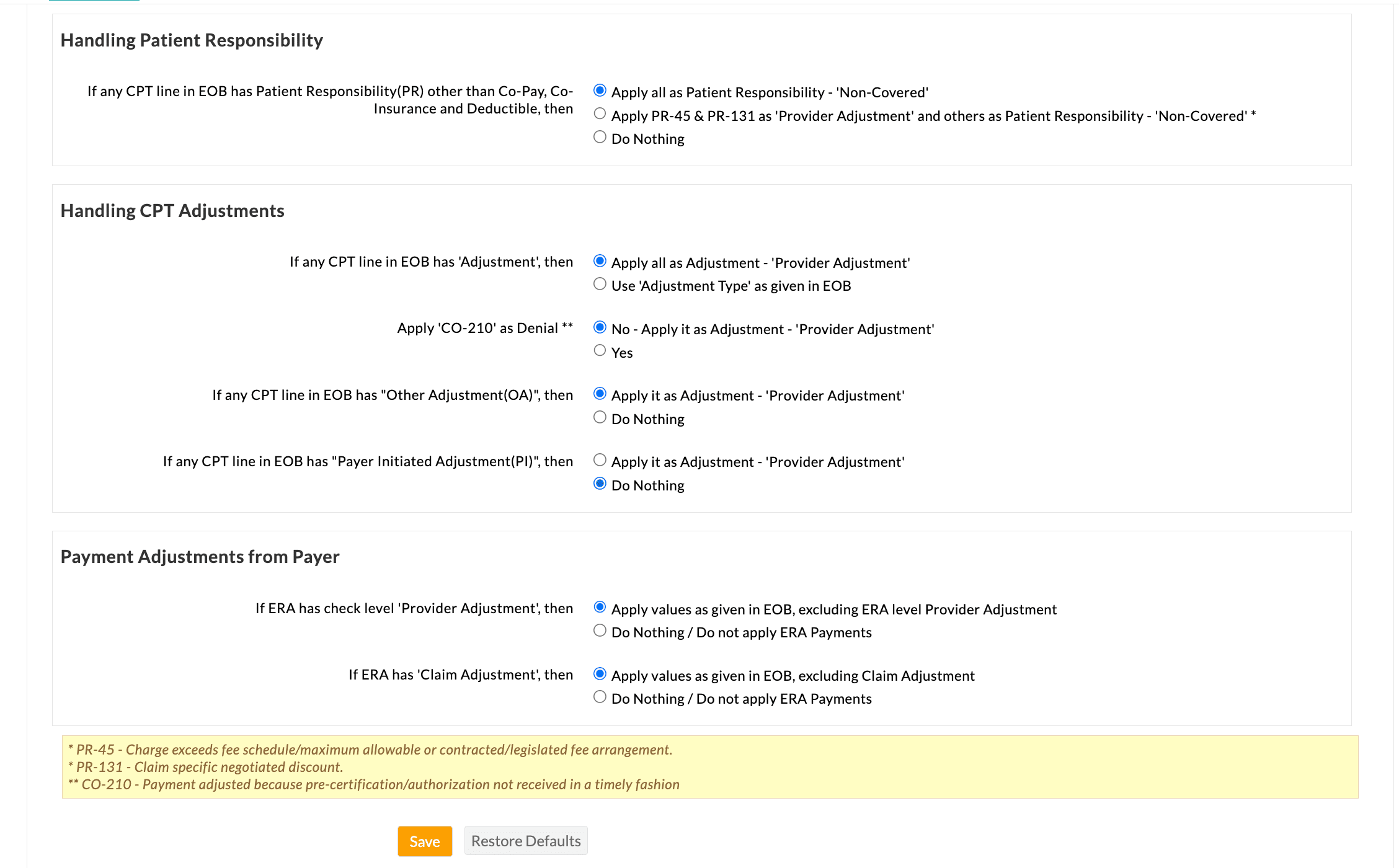
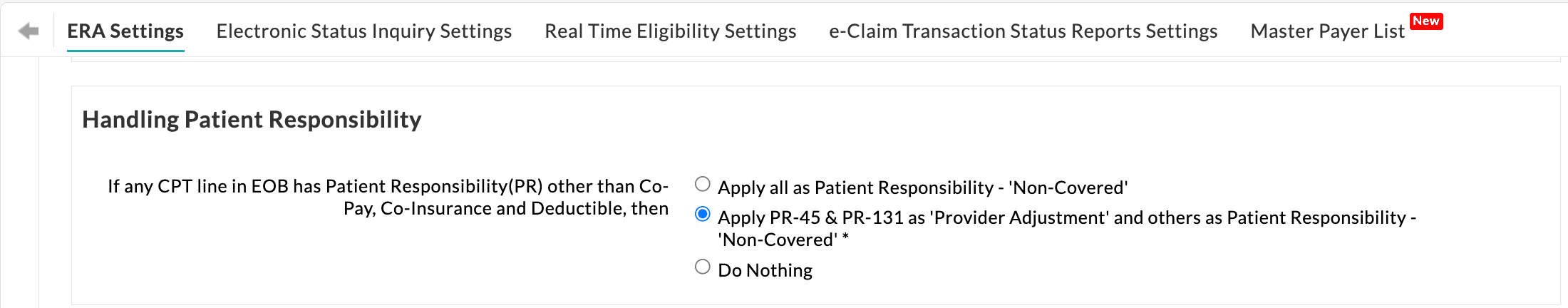
Handling Patient Responsibility
| If any CPT line in EOB has Patient Responsibility (PR) other than Co-pay, Co-insurance, and Deductible, then | The option 'Apply it as Patient Responsibility Not Covered' is selected by default, which marks the Patient Responsibility other than Copay, Co-insurance, and Deductible as Not Covered. |
| The option 'Apply PR-45 & PR-131 as 'Provider Adjustment' and others as Patient Responsibility - 'Non-Covered', marks the PR-45 and PR-131 codes as Provider Adjustment instead of Patient Responsibility and other PR codes as 'Non-Covered'. | |
| Select the 'Do Nothing' option if the above actions are not required. |
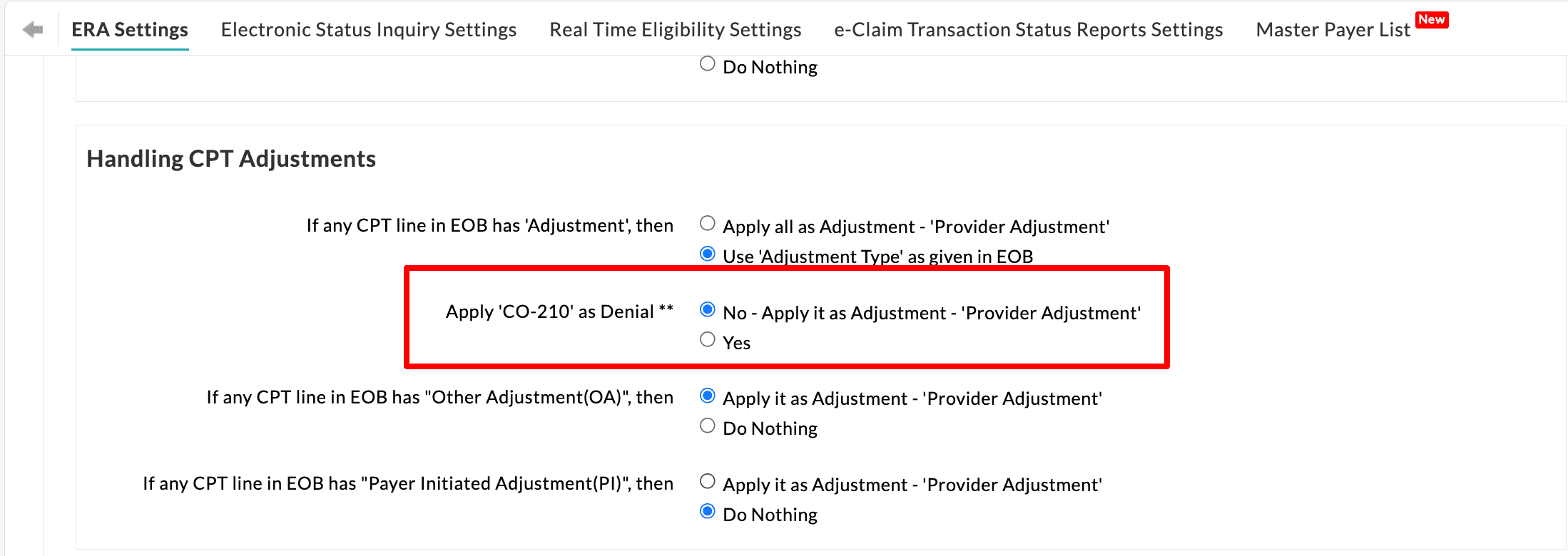
Handling CPT Adjustments
| If any CPT line in EOB has 'Adjustment', then | The option 'Apply all as Adjustment - Provider Adjustment' is selected by default, which marks all Adjustment types as Provider Adjustment with type Contractual Obligations.
The option 'Use 'Adjustment Type' as given in EOB' marks the Adjustment Type as received in the EOB. |
| Apply 'CO-210' as Denial | The default option, 'No - Apply it as Adjustment - Provider Adjustment', is selected to mark the CO-210 code as a Provider Adjustment.
Opting for 'Yes' will mark the CO-210 code as a denial, indicating that 'Payment adjusted because pre-certification authorization not received in a timely fashion' |
| If any CPT line in EOB has 'Other Adjustment', and if any CPT line in EOB has 'Payer Initiated Adjustment', then | The option 'Apply it as Adjustment - 'Provider Adjustment' is selected by default and marks Other Adjustment or Payer Initiated Adjustment in EOB as adjustment with type Contractual Obligations.
Select the 'Do Nothing' option if the above action is not required. |
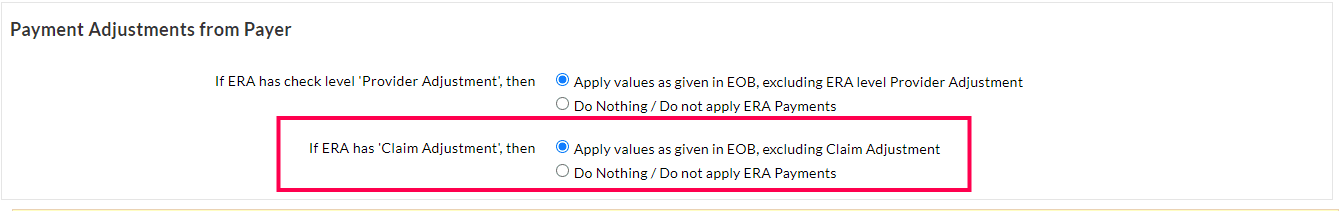
Payment Adjustments from Payer
| If ERA has check level 'Provider Adjustment', then | Sometimes, ERA may show Check-level Provider adjustments, which the biller will have to verify and adjust/apply against the respective Invoice. The option 'Apply values as given in EOB, excluding ERA level Provider Adjustment' ignores this check level Provider adjustment and applies payments received against each EOB to the respective claims.
Select the 'Do Nothing / Do not apply ERA Payments' option not to apply the payment if you need to verify and post it manually. |
| If ERA has 'Claim Adjustment', then | The option 'Apply values as given in EOB, excluding Claim Adjustment' ignores the Claim Adjustment and applies payments received against each EOB to the respective Claims.
The option 'Do Nothing / Do not apply ERA Payments' is chosen by default, which does not apply to the payment and allows you to verify and post it manually. |
Ability to Review the Applied ERA Payments
Upon downloading ERAs from the Clearinghouse, Charm automatically applies the ERA payments to corresponding Claims and marks them as reviewed.
However, for Practices that prefer to review ERA details and payments applied, Charm offers this capability, enabling them to retain control over the payment reconciliation process.
To enable manual review of ERA payments, follow the configuration steps outlined below.
- Navigate to 'Settings > Blling-eClaims > ERA Settings'.
- Ensure the 'Map EOB with Claim' and 'Apply Payments in EOB to the claim' settings are enabled.
- Choose 'No' for 'Review EOB Payments automatically' and click 'Save'.
- On enabling this setting, Practices can utilize the '# of Unreviewed EOBs' watchlist to filter ERAs that require manual review.
- On viewing the ERA, a 'Mark EOB as Reviewed' option will be shown against each EOB Payment, allowing Practices to review them.
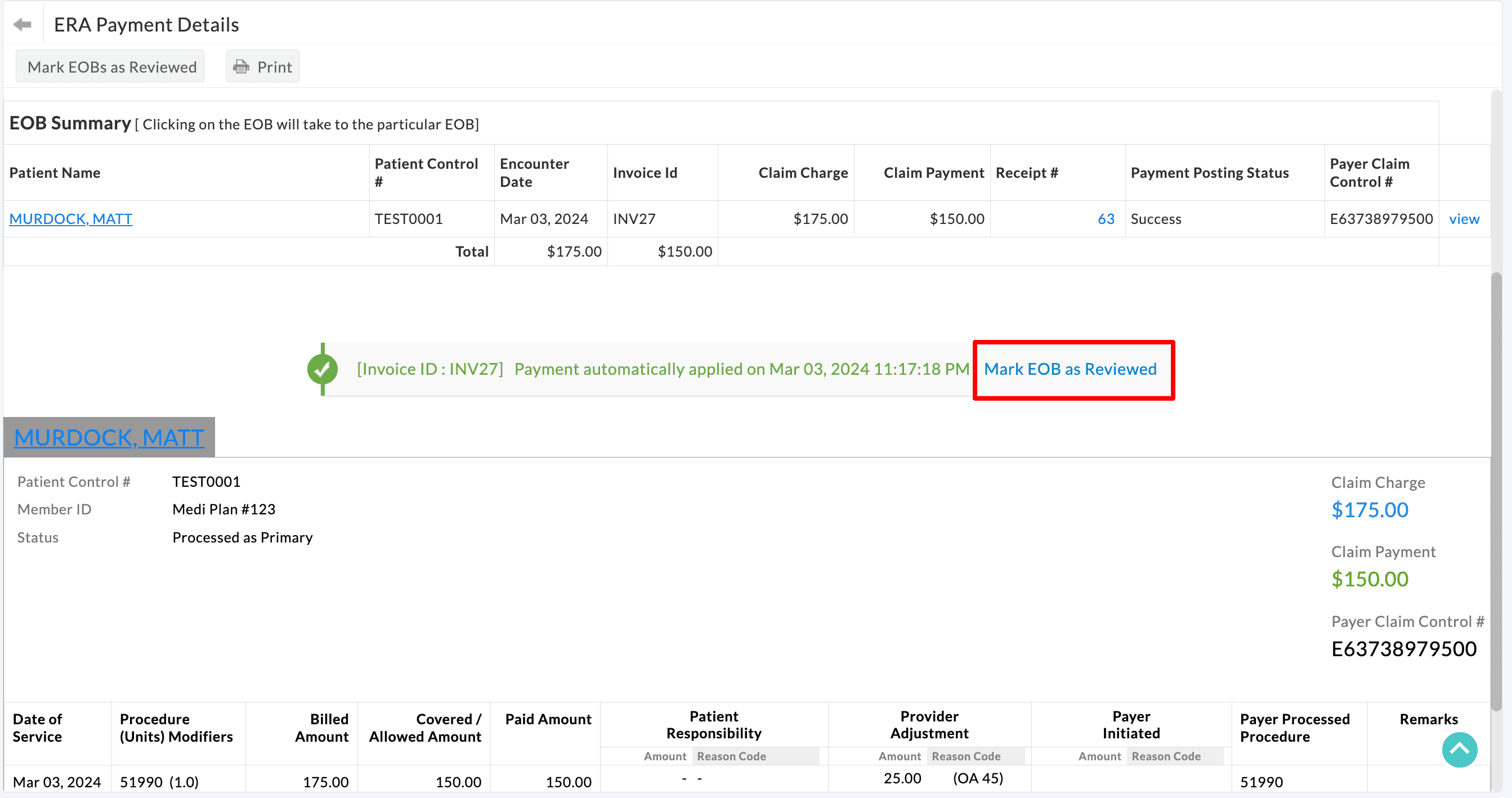
- Practices also have the option to review the entire ERA Payments at once by using the 'Mark EOBs as reviewed' button. Only EOB payments that are successfully applied can be reviewed.
Ability to Review the ERA and Initiate Payment Posting
Practices can review ERA payments before they are applied to Claims, gaining control over the payment reconciliation process. This will be particularly useful for Practices that prefer to apply payments only upon the realization of ERA payments.
By reviewing ERA payments in Charm, Practices can ensure that payments are reconciled accurately and aligned with their financial records.
To enable this option, follow the steps given below.
- Navigate to 'Settings > Billing-eClaims > ERA Settings'
- Choose 'Yes' for 'Map EOB with Claim'
- Choose 'No' for 'Apply Payments in EOB to the claim' and click 'Save'.
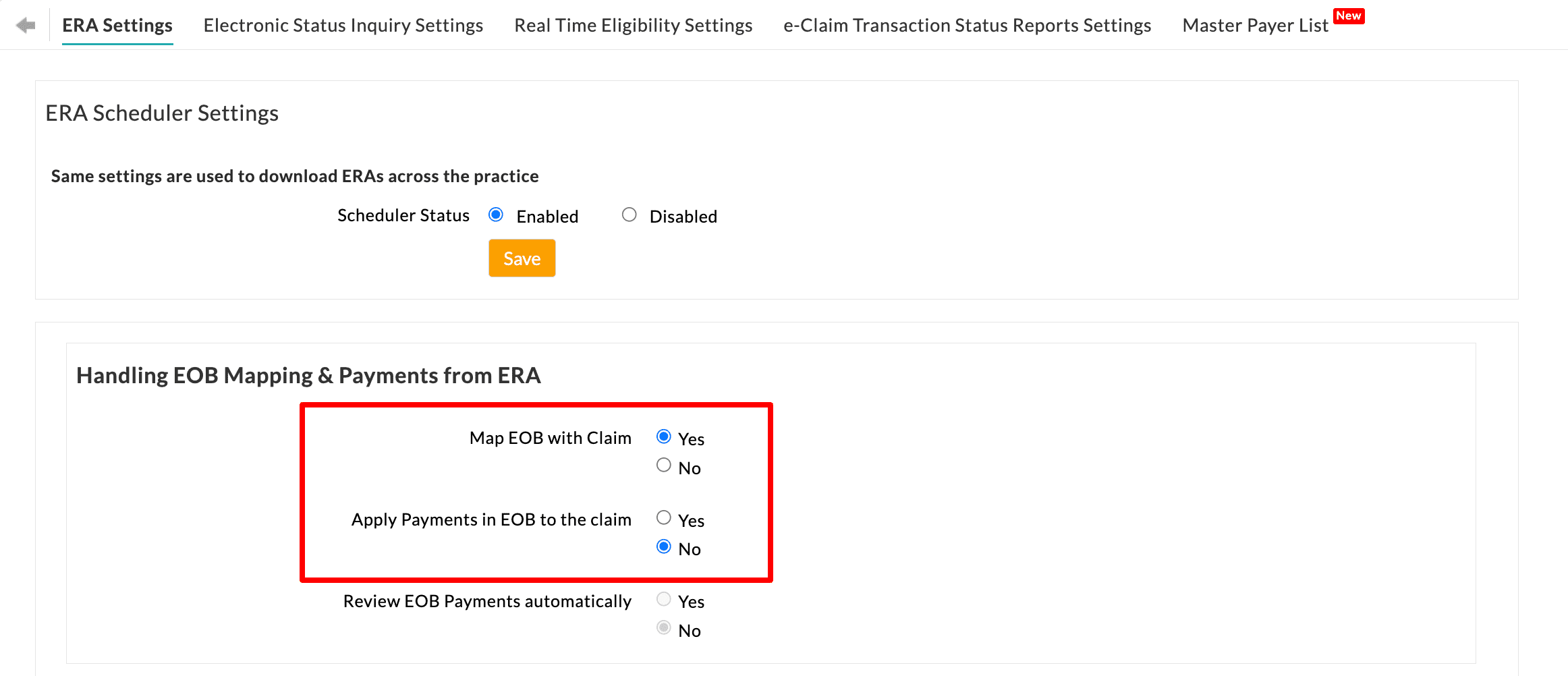
- On selecting 'No' for 'Apply Payments in EOB to the Claim', ERA payments will not be automatically applied upon downloading ERAs from Clearinghouse.
- Practices can now review and apply the ERA payments using the 'Apply EOB Payment' option, as shown below.
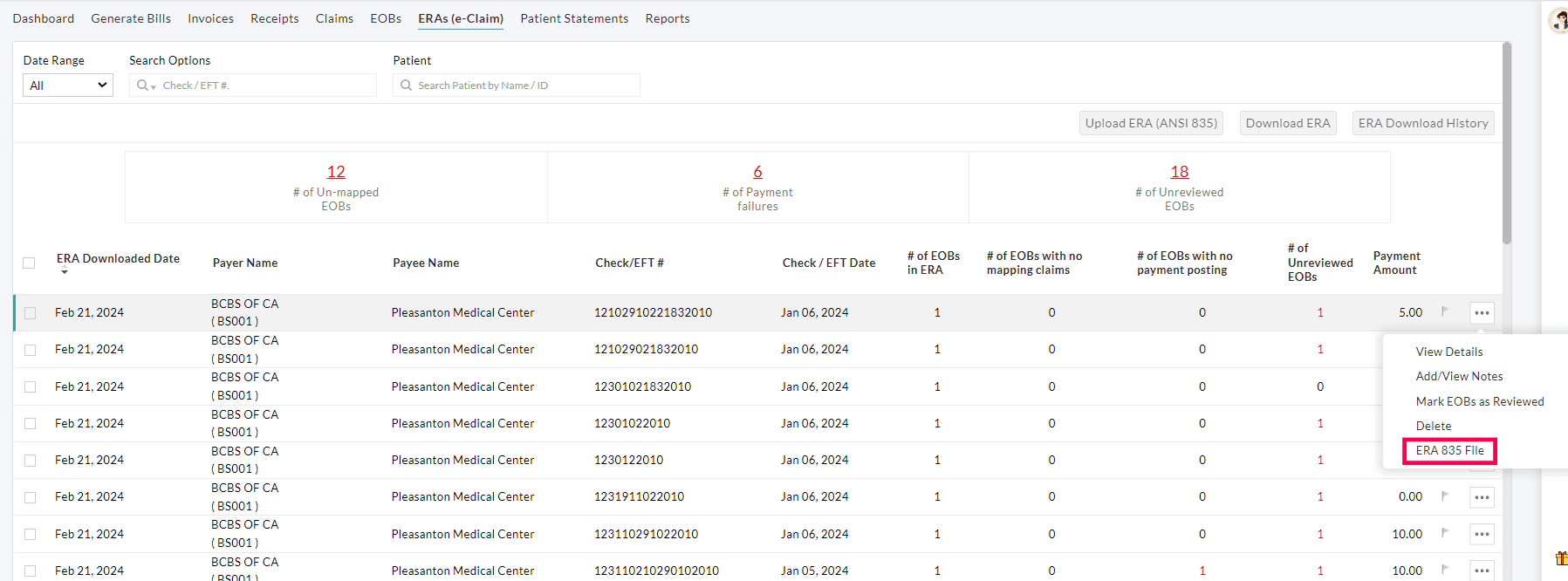
Option to Download 'ERA 835' File
Practices can use the 'Export ERA 835 File' option to download the ERA 835 files that Charm has received from the Clearinghouse. This option helps the Practices to reconcile payments received from the Payer.
To download the ERA 835 file, follow the steps given below.
- Go to 'Billing > ERAs (e-Claim)'
- Click the 'More Options' (...) icon against the downloaded ERA and select the 'ERA 835 FIle' option.
- The 835 file gets downloaded to the system.
Enhancements in ERA Payment Posting
We have added a few ERA rules in charm to handle ERA Payments better.
Option to Apply PR-45 and PR-131 as Provider Adjustment
When a Patient Responsibility other than Copay, Co-Insurance, and Deductible is posted from ERAs, it is automatically categorized as Non-Covered in Charm. However, practices now have the option to designate PR-45 and PR-131 as Provider Adjustment instead of marking them as Non-covered.
- PR-45 indicates that 'Charge exceeds fee schedule/maximum allowable or contracted/legislated fee arrangement'.
- PR-131 indicates 'Claim specific negotiated discount'
To enable this option, follow the steps given below.
- Navigate to 'Settings > Billing-eClaims > ERA Settings > Handling Patient Responsibility'.
- Choose 'Apply PR-45 & PR-131 as 'Provider Adjustment' and others as Patient Responsibility - 'Non-Covered' and click 'Save'.
Option to Apply CO-210 as Denial
Practices have the flexibility to designate CO-210 as a Denial in Charm.
CO-210 indicates the Payment got adjusted because pre-certification/authorization was not received in a timely fashion.
By specifically marking CO-210 as a Denial, Practices can readily identify and filter such Claims for further review and resubmission to the Payer.
Option to Apply payments even when ERA has 'Claim Adjustment'
Practices have the option to disregard the Claim Adjustment and apply payments received against each EOB to the respective Claims by choosing the 'Apply Values as given in the EOB' option.
Option to Use Adjustment Type as received from ERA
When posting ERA payments, all adjustments are automatically categorized as 'Provider Adjustments' by default. However, Practices now have the flexibility to utilize the Adjustment Type as received directly from the ERA.
Enabling this option allows Practices to identify the adjustment reasons accurately and their frequency, helping them to take necessary actions as needed based on this information.
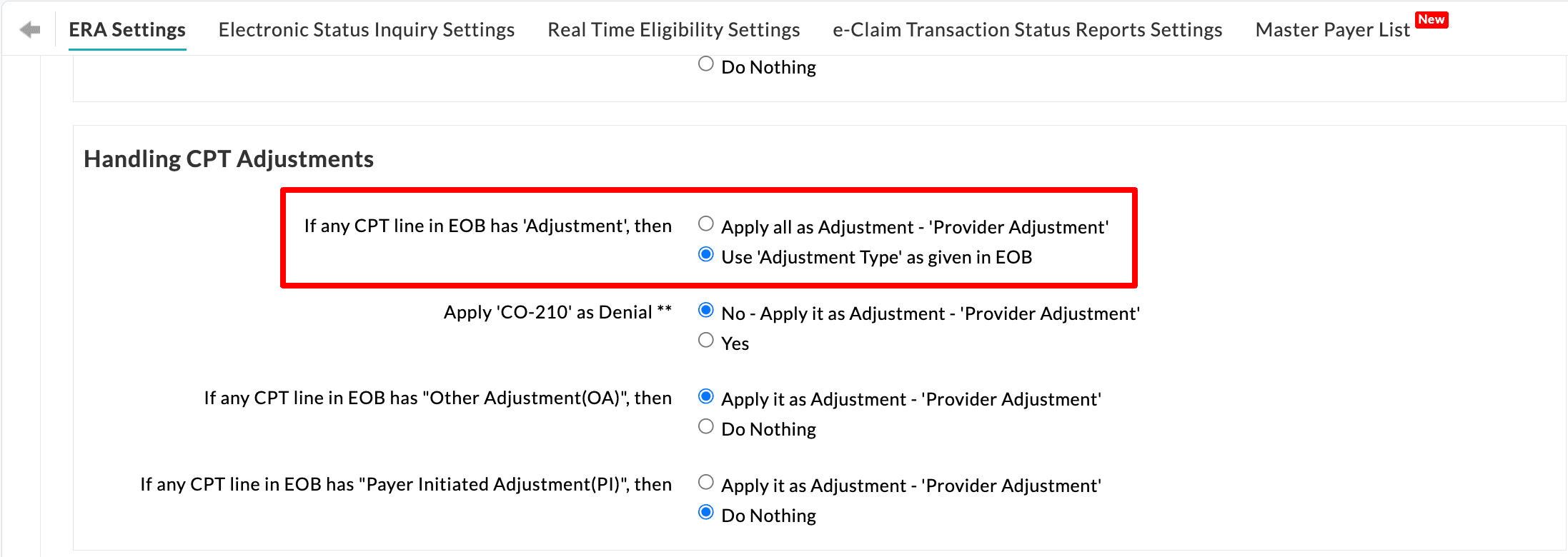
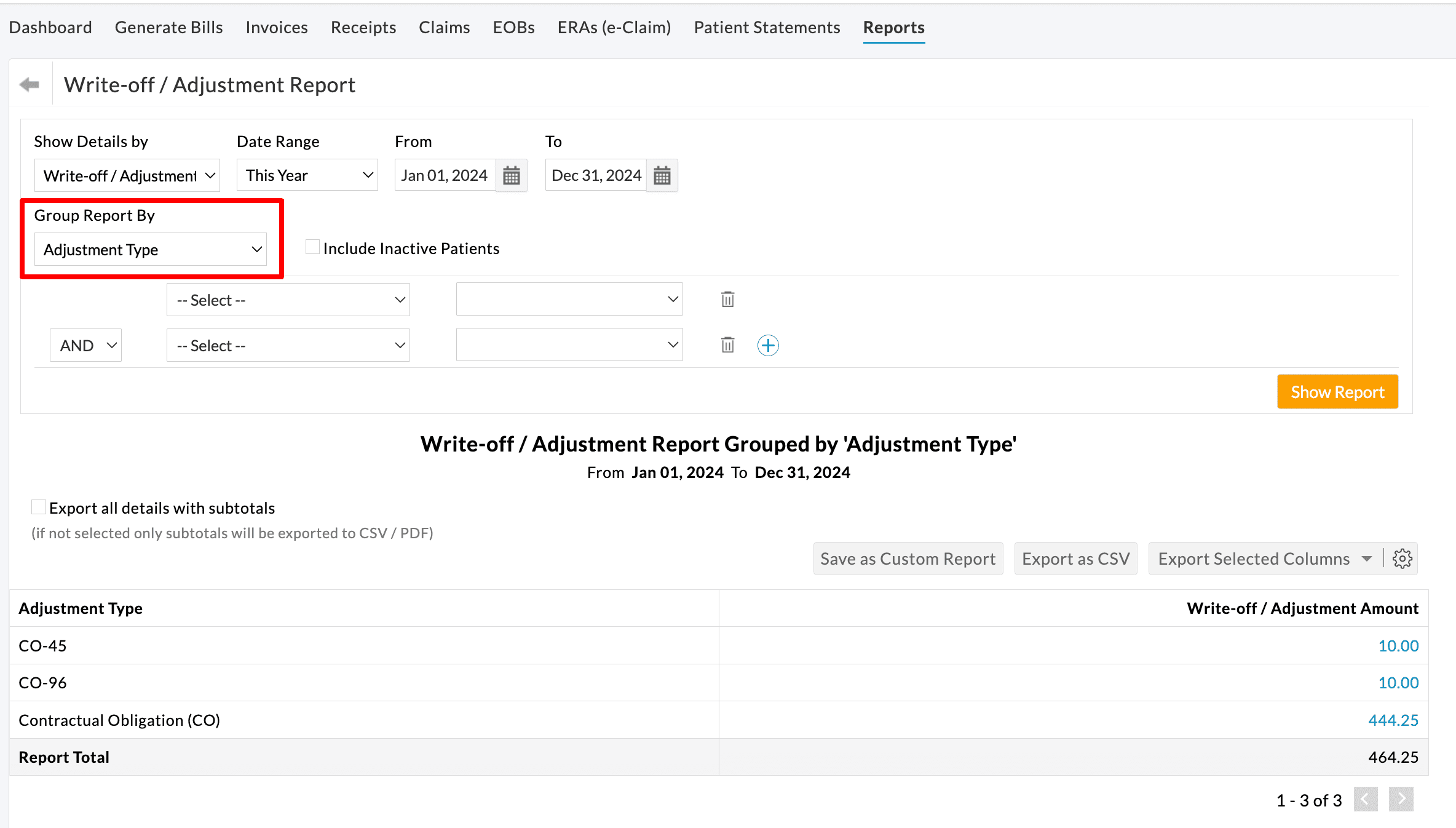
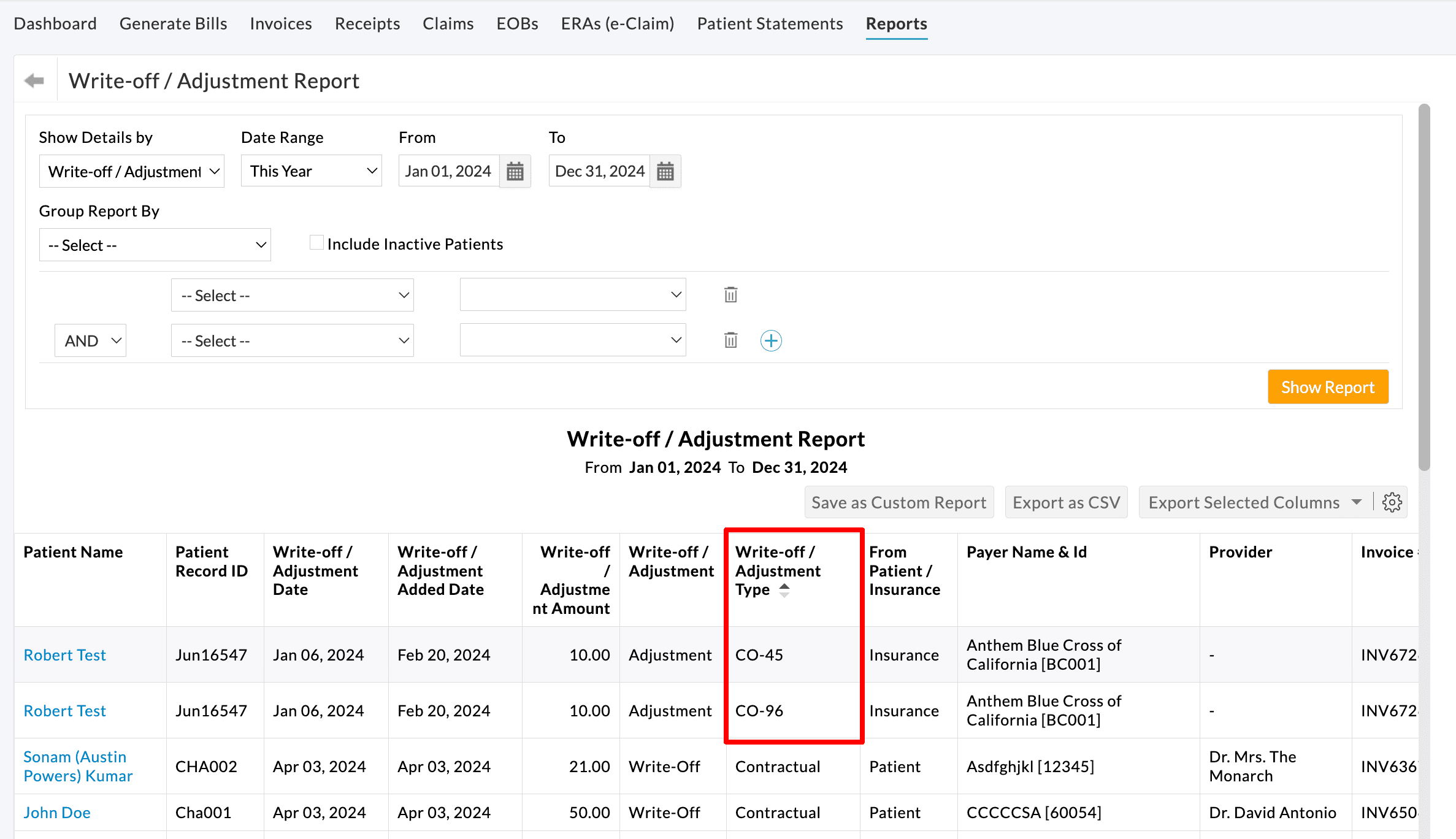
Practices can view the list of Adjustments received through ERA Payments under the 'Billing > Reports > Write-off / Adjustment Report' section.
On grouping the report based on 'Adjustment Type', all the adjustments received through ERAs will be listed, as shown below.
Enable Item Level Payments to Invoices
The EOB from the Payer has the Payment, Adjustment, and Patient Responsibility details for each line item in the Claim. It is also possible that one CPT in a Claim gets paid, while the other CPT gets denied.
It is recommended to enable line item level payments and get the payment & denial information from the Payer for individual CPT. To enable line item level payments, go to the 'Settings > Billing > Billing Settings > Invoice Settings' section and select 'Yes' for the 'Enable Item Level Payments for Invoices' option.

Configure Role-Based Access to ERA
Access to ERA and e-Claim submission are given to the Practice Admin and Biller roles by default. These permissions can also be given to other users using Role-Based Access in EHR.
Navigate to the 'Settings > Facility > Roles' section to grant or revoke permissions.
ERA Permissions
- View Only: To view the ERA tab under the Billing section.
- Download ERA (manual): For allowing members to download ERA manually.
- Manually map Claim to EOB: On granting this permission, the member can select the Claim for the EOB.
- Fixing payment failures: On granting this permission, the payment failure messages above the EOB can be dismissed by clicking the 'Do not show this message again' option.
- Export (PDF, Print): To enable the Print and Export to PDF options.

Delete an ERA
An option to delete an ERA from the list of ERAs is available under the 'Billing > ERAs(e-Claim)' section. Note that the payment applied to the Invoices or Claims in an ERA cannot be deleted. If required, the Practice can remove the payment applied to the Invoices.
- Go to 'Billing > ERAs(e-Claim)'
- Click the 'More Options' (...) icon against the ERA you need to delete.

- To delete multiple Invoices, select the Invoices and click the 'Delete ERA' button.

- A pop-up for confirmation gets opened. Click the 'Continue' button.

- If the payments are applied to the Invoices, an error message appears as shown in the screenshot below.
